Neurological disorders are among the most complex and costly to diagnose and manage, contributing billions in global healthcare expenditures each year.
By enhancing diagnostic accuracy, enabling early detection of conditions like Alzheimer’s and Parkinson’s, and optimizing patient triage and care pathways, AI empowers healthcare leaders to make informed decisions that boost both clinical outcomes and resource allocation.
Explore the top 12 AI for neurology use cases with real-life examples and key ethical considerations that healthcare providers and decision-makers must address when integrating these technologies.
AI for Neuro-oncology
Artificial intelligence (AI) is becoming an important tool in neuro-oncology, aiding in diagnosis, prognosis, and treatment planning for brain tumors. AI models, particularly machine learning (ML) and deep learning algorithms, enhance clinical practice by analyzing complex data, including medical images, patient records, and genomic information, to detect subtle abnormalities and refine treatment strategies.
Watch how AI is improving brain tumor diagnosis:
1. Brain tumor management
In brain tumor management, AI systems support clinical decision-making by improving MRI imaging, identifying tumor boundaries, and predicting treatment outcomes. Deep learning models, including artificial neural networks, aid in analyzing medical images and patient data to enhance diagnosis and prognosis.
AI algorithms help healthcare providers with treatment planning, from surgery to deep brain stimulation and drug discovery, contributing to more personalized treatment strategies.
According to a recent article, AI plays a role in brain tumor management across three major domains: diagnosis, prognosis, and therapeutic management (see Figure 1).
In diagnosis, AI enhances tumor detection and segmentation on MRI, enables rapid molecular classification during surgery, and combines data from multiple sources for greater accuracy.
For prognosis, AI models use radiomic and genetic markers to predict survival and recurrence more precisely than traditional methods.
In treatment, AI supports therapy planning by forecasting responses to radiation and chemotherapy, including the assessment of key biomarkers such as MGMT methylation.1
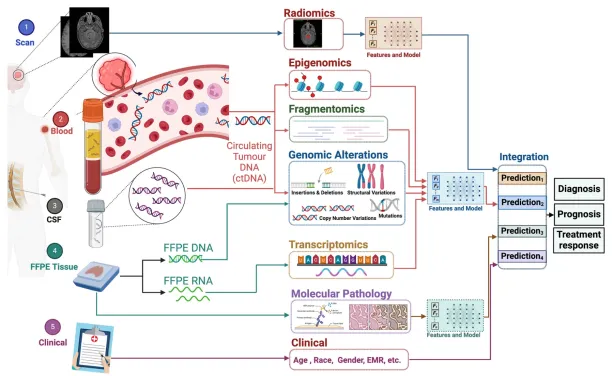
Figure 1: Graph showing how multimodal integration improves brain tumor diagnosis, prognosis, and treatment response prediction by combining diverse data types for more accurate analysis.
2. Healthcare data analysis in neuro-oncology
Beyond imaging, AI in neurology plays a role in natural language processing (NLP) for analyzing electronic health records and integrating AI into clinical trials. These AI models improve data quality and support clinical AI applications, enabling predictive models that support patient management.
AI-driven approaches also contribute to treating neurological disorders, including multiple sclerosis, acute stroke, and Alzheimer’s disease, by offering insights into disease progression and treatment responses.
AI for neuro-vascular diseases
AI has various applications for neurovascular disorders that can affect the blood supply in the brain or spinal cord. For instance, AI-enabled CT scanning for hemorrhagic patients allows automation of lesion segmentation and detection of hemorrhagic expansion.
One of the most common and dangerous neurovascular conditions is a stroke, globally ranking as the 2nd leading cause of death.2
Apart from the fatal outcomes, strokes can cause other serious complications for patients, including paralysis. AI can help treat patients who are affected by strokes by providing personalized treatments.
See how BrainQ and Google are working on an AI-enabled medical device that can help treat stroke patients:
3. Traumatic brain injury (TBI) detection
Traumatic brain injury (TBI) occurs when a sudden impact or force damages the brain, often due to accidents such as falls, sports injuries, or motor vehicle collisions. TBIs range from mild concussions to severe brain damage, leading to both short- and long-term health complications.
AI is playing a crucial role in improving TBI detection, diagnosis, and management. Machine learning algorithms and deep learning models analyze medical images, such as CT scans and MRI scans, to detect subtle abnormalities that might be missed by human observation. AI-powered tools can assess brain injuries, classify their severity, and predict potential complications.
NLP can also aid in TBI diagnosis by analyzing electronic health records and patient data to identify risk factors and inform more effective treatment planning. Healthcare providers may benefit from predictive models in determining personalized treatment strategies based on clinical data.
Additionally, AI models contribute to research in TBI-related neurological disorders, such as Alzheimer’s disease and stroke, by identifying patterns in large datasets.
According to a recent study by the University of Cambridge and Imperial College London, AI can be used to successfully and accurately scan medical images and detect different types of brain injuries.3
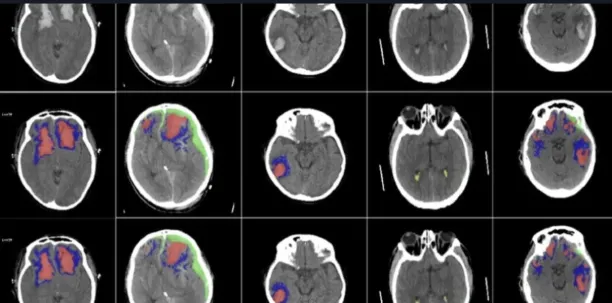
Figure 2: An example of brain scans with AI for early diagnosis.
4. Reducing overuse of medical imaging
Overuse of medical imaging is another problem in pediatric TBI. Even when a mild injury happens, precautionary CT scans are performed on the child to understand the severity of the damage, and only 10% of these scans end up finding TBI.4
In other words, 90% of the time, the child is needlessly exposed to radiation caused by medical imaging, with the latter producing nothing of significance.
According to a recent study, deep neural networks can predict the need for CT scans in mild pediatric TBI, thereby reducing the overuse of medical imaging and unnecessary exposure to radiation.5
AI for neurosurgery
Neurosurgery or brain surgery is one of the riskiest and most complicated medical procedures in the field of medicine. Even the most experienced surgeons can make various types of errors and mistakes that can have serious consequences and lead to future health issues for the patient.
AI can help improve the pre-operative, intra-operative, and post-operative phases of brain surgery:
5. Preoperative planning & diagnosis
- Medical imaging analysis: AI aids in the more accurate interpretation of MRI, CT, and PET scans by identifying tumors, aneurysms, and vascular abnormalities with greater speed and accuracy than traditional methods. This reduces diagnostic errors and helps in early disease detection.
- Automated segmentation: AI-powered segmentation tools accurately delineate brain structures, lesions, and blood vessels, enabling precise mapping of pathological areas. This aids neurosurgeons in planning optimal surgical approaches while minimizing damage to critical brain regions.
- Predictive analytics: Machine learning models analyze patient data to predict disease progression, such as glioblastoma growth, stroke risk, or the progression of neurodegenerative disorders. These predictive insights enable the tailoring of personalized treatment strategies.
6. Intraoperative Assistance
- Robot-assisted surgery: AI-powered robotic platforms assist in performing minimally invasive procedures with high precision, reducing human error and improving patient safety.
- Augmented Reality (AR) & AI integration: AI enhances AR overlays that project imaging data onto the surgical field, providing real-time guidance on brain structures and tumor margins. This increases accuracy during complex neurosurgical procedures.
- AI-guided microsurgery: AI enhances microsurgical precision by providing real-time feedback on tissue characteristics and instrument positioning. It can differentiate between healthy and diseased tissues, ensuring safer resection and reduced collateral damage.
Real-life example: The ROSA (Robotic Surgical Assistant)
The ROSA (Robotic Surgical Assistant) technology, developed by Zimmer Biomet and incorporating Stäubli’s six-axis robotic arm, is an FDA-approved surgical robot utilized in over 200 hospitals worldwide.
Designed by surgeons for surgeons, ROSA offers an integrated navigation platform that increases precision in various surgical procedures, including those involving the spine and brain.
ROSA’s key features include:
- Dynamic tracking: The system comprises two mobile units positioned adjacent to the operating table. One unit is equipped with a camera that continuously monitors the robotic arm’s movements in three dimensions, enabling real-time adjustments during surgery.
- Six degrees of freedom: The Stäubli robotic arm offers six degrees of freedom, enabling precise, multidimensional movements that mimic the dexterity of a human hand. This capability is crucial for accessing complex anatomical structures with high accuracy.
- Minimally invasive surgery support: ROSA facilitates minimally invasive procedures by allowing surgeons to operate through smaller incisions. This approach reduces patient trauma and accelerates recovery times.
By integrating advanced robotics with surgical expertise, ROSA technology represents a significant advancement in surgical assistance, aiming to improve patient outcomes and increase the precision of complex surgical interventions.6

Figure 3: An example from ROSA robotic surgical system by Zimmer Biomet, designed for precise neurosurgical procedures.
Real-life example: Mazor X Stealth Edition Robotic Guidance Platform
On June 24, 2022, spine surgeons at University Orthopedics in East Providence, Rhode Island, achieved a significant milestone by performing the state’s first minimally invasive spine surgery using the Mazor X Stealth Edition Robotic Guidance Platform.
The Mazor X Stealth Edition Platform enables surgeons to develop and execute personalized 3D surgical plans for each patient prior to entering the operating room.
During surgery, the system’s robotic arm maintains the precise positioning of instruments, allowing surgeons to make accurate micro-incisions with robotic guidance. This technology aims to increase surgical precision, reduce recovery times, and shorten hospital stays.7
7. Postoperative care & outcome prediction
- Patient monitoring: AI-driven systems analyze continuous physiological data from ICU patients, detecting complications like cerebral edema, hemorrhage, or increased intracranial pressure. Early warnings enable prompt intervention, improving survival rates.
- AI-based rehabilitation: Machine learning models assess patient progress and predict recovery trajectories, allowing for personalized rehabilitation plans. AI-driven neurorehabilitation tools help in motor and cognitive recovery, particularly after stroke or traumatic brain injury.
8. Neuromodulation & Brain-Machine Interfaces (BMI)
- Deep Brain Stimulation (DBS): DBS with AI improves efficacy while minimizing side effects by optimizing electrode placement and stimulation parameters for neurological disorders like Parkinson’s, epilepsy, and depression.
- Brain-Computer Interfaces (BCI): AI deciphers neural signals, enabling paralyzed patients to control prosthetic limbs, communicate via thought-based interfaces, or interact with smart devices.
9. AI in neurosurgical education & simulation
- Virtual Reality (VR) & AI for training: AI-powered forms of virtual reality simulations allow neurosurgeons to practice complex procedures in a controlled environment, improving surgical skills without risk to patients.
- Decision support systems: AI-driven tools provide real-time recommendations during surgery by analyzing vast amounts of medical data, helping neurosurgeons make critical intraoperative decisions with greater confidence.
Molecular analysis and biomarker discovery for neurological disorders
10. AI in molecular pathology and genomic analysis
AI supports molecular pathologists by analyzing complex biological data, including:
- Mutation patterns: AI-driven tools analyze DNA sequences to identify mutations associated with neurological disorders, including genetic mutations in amyotrophic lateral sclerosis (ALS), Huntington’s disease, and Parkinson’s disease.
- RNA sequencing analysis: AI models process transcriptomic data to identify differentially expressed genes in neurological conditions like multiple sclerosis (MS) and Alzheimer’s disease (AD).
11. Biomarker discovery
Biomarkers are measurable indicators of biological processes and disease states. AI helps with biomarker discovery by:
- Identifying early disease markers: AI detects biomarkers from genomic, proteomic, and metabolomic data, enabling the early diagnosis of conditions such as Parkinson’s, epilepsy, and brain tumors.
- Predicting treatment response: AI models analyze biomarkers to predict how patients will respond to therapies, such as immunotherapy in multiple sclerosis or precision medicine in epilepsy.
12. Molecular diagnostics for neurological diseases
AI-powered molecular diagnostics aid in diagnosing and monitoring various neurological disorders:
- Alzheimer’s Disease: AI analyzes blood-based and cerebrospinal fluid (CSF) biomarkers, such as amyloid-beta and tau proteins, to increase early detection and disease progression monitoring.
- Multiple Sclerosis (MS): AI identifies molecular signatures that help distinguish between MS subtypes and predict responses to disease-modifying therapies.
- Rare neurological diseases: AI accelerates the diagnosis of rare genetic disorders by analyzing whole-genome sequencing (WGS) data to identify causative mutations.
Ethical concerns and future directions
| Ethical Considerations | How to Handle Them |
|---|---|
| Data Quality | Collect diverse, standardized, and validated datasets |
| Bias in Training Data | Identify gaps, use bias detection tools, and adjust for demographic diversity |
| Fairness in Predictions | Train on balanced data, apply fairness algorithms, and monitor outputs regularly |
| Clinical Relevance | Collaborate with clinicians to ensure alignment with medical needs |
| Health Equity | Design inclusive models and ensure equitable access to AI tools |
| Use of Generative AI/LLMs | Support clinical decisions and personalize care, especially for rare conditions |
| Ethical Governance | Establish strong data governance and ensure transparency and accountability |
The integration of AI in neurological diseases raises concerns regarding data governance, ethical considerations, and the assessment of clinical outcomes. As AI systems rely on large datasets, ensuring high-quality input data and addressing biases in the training data are crucial for developing reliable clinical applications.
High-quality input data can be achieved by:
- collecting diverse and well-documented datasets,
- standardizing data collection methods,
- and implementing thorough validation processes.
Utilizing multiple data sources, including electronic health records, imaging scans, and genetic information, can enhance the accuracy of AI-driven insights.
To address biases in training data, it is essential to:
- identify gaps in representation,
- apply bias detection tools,
- and adjust datasets to reflect the diversity of patient populations.
Training AI models with balanced data from diverse demographic groups, incorporating fairness-focused algorithms, and regularly evaluating model outputs can help mitigate disparities in clinical predictions.
Ongoing collaboration between healthcare professionals and data scientists is crucial to ensure that AI systems align with clinical needs and do not perpetuate existing healthcare inequalities.
Generative AI models and large language models have the potential to support healthcare providers further, assist in analyzing medical images, and contribute to the development of personalized treatment strategies for rare neurological disorders.
By prioritizing accurate data collection and ethical AI development, these technologies can enhance diagnostic precision, improve treatment recommendations, and lead to better outcomes for patients with neurological conditions.
External Links
- 1. Artificial intelligence in neuro-oncology: advances and challenges in brain tumor diagnosis, prognosis, and precision treatment | npj Precision Oncology. Nature Publishing Group UK
- 2. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6288566/
- 3. https://www.thelancet.com/journals/landig/article/PIIS2589-7500(20)30085-6/fulltext
- 4. ScienceDirect.
- 5. https://www.jacr.org/article/S1546-1440(22)00247-2/fulltext
- 6. https://www.staubli.com/global/en/robotics/industries/medical-robotics/first-robotic-platform-for-surgical-assistance.html
- 7. https://blog.universityorthopedics.com/university-orthopedics-surgeons-perform-first-successful-spine-surgery-in-ri-using-mazor-x-stealth-edition-robotic-guidance-platform/


Comments
Your email address will not be published. All fields are required.